Does Arch Pain Need Surgical Procedures ?
Flat feet and fallen arches are terms used to describe lowering of the long inner arch of the foot. In the past, we thought that flat feet were a sign of a poorly developed or poorly structured foot. Now we know that people with flat feet function generally well and that flat feet don?t cause many foot problems. The most important factor in foot soreness and injury is not how flat or high your arches are, but the way you walk and move. If your feet move abnormally while you are walking or standing, this can make you more prone to injuries and foot soreness.
Causes
Over-stretching or tearing the arch pad causes the dull ache that is associated with arch pain. Pain is most keenly felt when weight is put onto the foot, or when pushing off the foot into the next stride. The pain of foot arch strain can be particularly acute after sitting for a long time, or when getting up in the morning. Those most susceptible to the condition are people with very high, rigid arches. The injury is also common in middle-aged people who have been inactive for a long period of time before suddenly increasing their physical activity. The injury is particularly common in runners and joggers.
Symptoms
Persistant pain and selling under the ball of the foot and extending towards the toes (most commonly the 2nd). Some swelling may be disable on the top of the foot along with redness. Often a sensation of 'walking on the bones for the foot' will be described, and there is a positive Lachman's test. Often a tear will result in the toes splaying (daylight sign) and clawing.
Diagnosis
Diagnosis of a plantar plate tear can often be challenging due to the complex nature of the anatomy of the foot. Careful history taking and an examination of the area of pain is required to determine the extent and cause of the tear. If necessary, further investigations such as x-rays or diagnostic ultrasound may be ordered by your podiatrist to help evaluate the severity of the problem.
Non Surgical Treatment
When you first begin to notice discomfort or pain in the area, you can treat yourself with rest, ice, compression, and elevation (RICE). Over-the-counter medications may also be used to reduce discomfort and pain. Rest will allow the tissues to heal themselves by preventing any further stress to the affected area. Ice should be applied no longer than 20 minutes. The ice may be put in a plastic bag or wrapped in a towel. Commercial ice packs are not recommended because they are usually too cold. Compression and elevation will help prevent any swelling of the affected tissues. There are two types of over-the-counter medication that may help with the pain and swelling of arch pain. Acetaminophen (Tylenol) will help with the pain, and a nonsteroidal anti-inflammatory such as aspirin, ibuprofen, or naproxen will help with the pain and battle the inflammatory response. Caution should be taken when using these drugs, and dosage should not exceed the labeled directions. Special care should be taken and a physician consulted if you have a history of stomach ulcers. Those who have chronic medical conditions or who are taking other medications should consult with their doctor regarding the most appropriate type of pain and/or anti-inflammatory medications. Commercial over-the-counter arch supports or orthotics may also help to ease arch pain.

Surgical Treatment
There are two types of bone procedure for flat feet, those where bone cuts and bone grafts are used to alter the alignment by avoiding any joint structures, or joint invasive procedures (called fusions or arthrodeses) that remove a joint to reshape the foot. With joint fusion procedures, there are those procedures that involve non-essential joints of the foot versus those that involve essential joints. All bone procedures have their place in flat foot surgery, and Dr. Blitz carefully evaluates each foot to preserve as much motion and function while obtaining proper and adequate alignment. In many cases a flat foot reconstruction involves both soft tissue procedures and bone procedures to rebuild and restore the arch. There are several joints in the arch of the foot that can collapse - and these joints are non-essential joints of the foot. This does not mean that they do not have a purpose, but rather become inefficient is providing a stable platform for function. As such, locking these non-essential non-functioning joints into place is commonly recommended. These joints are fused together with screws and/or plates. A heel bone that is no longer in proper position and pushed outwards away from the foot can be corrected with a bone cut and realignment procedure, so long as the displacement is not too significant. A benefit of this surgery is that it keeps the back portion of the foot mobile, and helps the surrounding tendons work for efficiently in maintaining the arch. In certain flat feet, the foot is deviated outwards and away from the midline of the body. Sometimes, this is due to the outer portion of the foot being shorter than the inner portion. Here bone graft can be added to the outer edge of the foot to lengthen the foot to swing the foot over into a corrected position. This procedure is most commonly performed in children and young adults. A bone graft is inserted into the top part of the arch to realign a component of the flat foot, medically known as forefoot varus or medial column elevatus. The back part of the foot (called the rearfoot complex) can be the cause (or source) of the flat foot or the simply affected by the flat foot foot. In simple terms, the back part of the foot can be made to flatten out due to arch problems - and vica versa for that matter. Dr. Blitz specifically identifies the cause of the flat foot as this will determine the best treatment plan, as each flat foot needs to be evaluated individually. The rearfoot is made up of three joints, and depending on the extent and most importantly the rigidity of these joints, they may require fusion to restore alignment. When all three joints require fusion - this call is a triple arthrodesis. For completeness, isolated fusion of any of the three joints can be performed (such as subtalar joint arthrodesis, talonavicular arthrodesis, and calcaneaocuboid joint arthrodesis). The medical decision making for isolated fusions is beyond the scope this article, but Dr. Blitz tries to avoid any rearfoot fusion for flexible feet because these are joints are essential joints of the foot, especially in younger people. Those in severe cases, it may be advantageous to provide re-alignment.
Prevention
It is possible to prevent arch pain by wearing well-fitting shoes while performing any physical activity. Many times doctors will suggest a therapeutic shoe with a higher heel to relieve the pressure on the achilles tendon and also the arch muscle (plantar fasciitis). People with arch pain suffer from regular flare-ups of pain. However there is no risk to others as this is not a contagious condition.
Stretching Exercises
Flexibility is important in preventing injuries. With a simple stretching exercise, you can rehabilitate the muscles of your foot to relieve arch pain and prevent future injuries. This simple exercise by Tammy White and Phyllis Clapis for Relay Health is a good way to strengthen your foot muscles and stretch your plantar fascia. Sit in a chair and cross one foot over your other knee. Grab the base of your toes and pull them back toward your leg until you feel a comfortable stretch. Hold 15 seconds and repeat three times. When you can stand comfortably on your injured foot, you can begin standing to stretch the plantar fascia at the bottom of your foot.
Posterior Tibial Tendon Dysfunction Symptoms
Overview
Posterior Tibial Tendon Dysfunction (PTTD) is a painful flatfoot condition that affects adults, primarily over the age of 50. Also known as Adult Acquired Flatfoot, this issue affects women more than men and is linked to obesity, hypertension and diabetes. Most people with PTTD have had flat feet all of their lives. Then, for reasons not fully understood, one foot starts to become painful and more deformed. 
Causes
As the name suggests, adult-acquired flatfoot occurs once musculoskeletal maturity is reached, and it can present for a number of reasons, though one stands out among the others. While fractures, dislocations, tendon lacerations, and other such traumatic events do contribute to adult-acquired flatfoot as a significant lower extremity disorder, as mentioned above, damage to the posterior tibial tendon is most often at the heart of adult-acquired flatfoot. One study further elaborates on the matter by concluding that ?60% of patients [presenting with posterior tibial tendon damage and adult-acquired flatfoot] were obese or had diabetes mellitus, hypertension, previous surgery or trauma to the medial foot, or treatment with steroids?.
Symptoms
Many patients with this condition have no pain or symptoms. When problems do arise, the good news is that acquired flatfoot treatment is often very effective. Initially, it will be important to rest and avoid activities that worsen the pain.
Diagnosis
Looking at the patient when they stand will usually demonstrate a flatfoot deformity (marked flattening of the medial longitudinal arch). The front part of the foot (forefoot) is often splayed out to the side. This leads to the presence of a ?too many toes? sign. This sign is present when the toes can be seen from directly behind the patient. The gait is often somewhat flatfooted as the patient has the dysfunctional posterior tibial tendon can no longer stabilize the arch of the foot. The physician?s touch will often demonstrate tenderness and sometimes swelling over the inside of the ankle just below the bony prominence (the medial malleolus). There may also be pain in the outside aspect of the ankle. This pain originates from impingement or compression of two tendons between the outside ankle bone (fibula) and the heel bone (calcaneus) when the patient is standing.
Non surgical Treatment
Conservative treatment also depends on the stage of the disease. Early on, the pain and swelling with no deformity can be treated with rest, ice, compression, elevation and non-steroidal anti-inflammatory medication. Usually OTC orthotic inserts are recommended with stability oriented athletic shoes. If this fails or the condition is more advanced, immobilization in a rigid walking boot is recommended. This rests the tendon and protects it from further irritation, attenuation, or tearing. If symptoms are greatly improved or eliminated then the patient may return to a supportive shoe. To protect the patient from reoccurrence, different types of devices are recommended. The most common device is orthotics. Usually custom-made orthotics are preferable to OTC. They are reserved for early staged PTTD. Advanced stages may require a more aggressive type orthotic or an AFO (ankle-foot orthosis). There are different types of AFO's. One type has a double-upright/stirrup attached to a footplate. Another is a gauntlet-type with a custom plastic interior surrounded be a lace-up leather exterior. Both require the use of a bulky type athletic or orthopedic shoes. Patient compliance is always challenging with these larger braces and shoes. 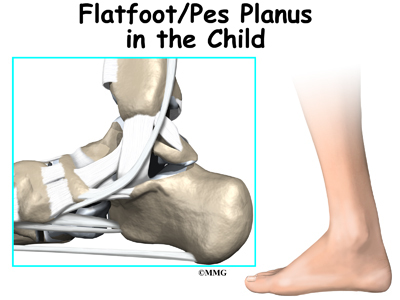
Surgical Treatment
Flatfoot reconstruction (osteotomy). This is often recommended for flexible flatfoot condition. Flatfoot reconstruction involves cutting and shifting the heel bone into a more neutral position, transferring the tendon used to flex the lesser toes (all but the big toe) to strengthen the posterior tibial tendon, and lengthening the calf muscle. Fusion (also known as triple arthrodesis). Fusion involves fusing, or making stiff, three joints in the back of the foot the subtalar, talonavicular, and calcaneocuboid joints, to realign the foot and give it a more natural shape. Pins or screws hold the area in place until it heals. Fusion is often recommended for a rigid flatfoot deformity or evidence of arthritis. Both of these surgeries can provide excellent pain relief and correction.